Injury Management: Psychosocial Influences on Recovery and Return to Work
Author: Lauren Barrett // Rehabilitation Professional
This article will provide a description of the psychosocial factors involved in the injury management system, explaining what the role of each factor is, and why they are so important on recovery and injury management.
When assisting a person to return to work following an injury related absence, it’s important to consider the other factors which may impact on an injured person’s recovery and reintegration to the workplace – factors that go beyond the injury itself.
While working in injury management as both a treating psychologist and a rehabilitation consultant, it has been my experience that when an injury is considered in isolation recovery and return to work is often delayed due to the impact of other stressors that have occurred in relation to the injury. In turn this delay in recovery may bring on additional stressors and a person can fall victim to a cycle of distress and delayed recovery.
You might ask then, what are these stressors and what are psychosocial factors? Why are they so important when considering injury management?
What are the Psychosocial factors?
Psychosocial refers to the influence of psychological, social, cultural, and environmental phenomenon on human functioning and behaviour. These factors occur in every aspect of life, from family dynamics in the home to social interaction in the workplace; from access to health care and having basic housing and financial stability.
Psychosocial factors are a significant determinant in recovery and overall wellbeing. Physical and psychological health don’t function in a vacuum and instead, they are influenced by internal and external stressors that, on the surface, often seem unrelated.
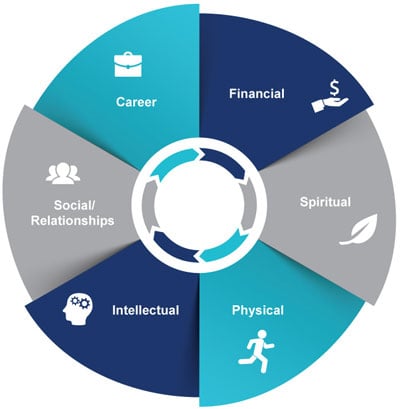
The diagram below displays different psychosocial factors in a wheel – it is not an exhaustive list of factors, but some of the major categories for consideration. A wheel is a great symbol for the psychosocial factors involved in the injury management system and makes it easier to identify the different facets of life as a whole, rather than as individual slices of pie.
Below I’ll highlight some of the psychosocial factor’s I’ve seen during my experience in helping people recover from both psychological and physical injuries (though I won’t be able to cover all of these), and I invite you to reflect on your own experiences and see if you are able to identify times where something external to an injury or illness impacted on recovery.
1. A Psychosocial Workplace
Our day to day environment is a strong determinant of our wellbeing. We’ve all had those mornings where we’ve woken up and just wanted to go back to bed, but have we really stopped to think about what made us actually push through and go to work?
You might say “I go to work because I love my job” or you might respond more along the lines of: “I have to go to work, I need the money!”. Both of these answers reflect the influence of psychosocial factors.
Imagine: When you get to work in the morning, you’re five minutes late, you’re shaking. Your boss pulls you aside and tells you that this is unacceptable, that you should have left home earlier. You try to explain. You try to say that you left home an hour ago (the trip normally takes 30 minutes), you dropped your toddler at pre-school and then you were stuck in traffic due to a car accident. Your boss doesn’t listen.
You go to your desk and try to get through the day, wondering why you come to work when you feel so unsupported. You think again of your toddler, you think of how important it is to get paid to be able to afford food and a roof over your head.
Now imagine that you’ve suffered an injury. Imagine trying to return to this workplace, what goes through your mind?
2. Interpersonal or Social Factors
Social influences both at work and at home play a significant part in recovery from injury or return to work following a prolonged absence.
In the injury management, appropriate social support is important for general human wellbeing and recovery from injury. We are by nature, social animals and where a person is supported, they are likely to experience less emotional and psychological distress, have increased self-esteem and even experience physiological benefits! In cases where support is absent, a person is likely to feel isolated and lonely, they may experience increased risk of physical and psychological illnesses.

Recovery and return to work can also be impacted by negative social relationships – like in our example above with the boss who wouldn’t listen. Following an injury (physical, or psychological) returning to an unsupportive workplace can be an insurmountable task. The feeling of dread in the morning and the ongoing avoidance reinforce the negative relationship, reinforce the distress and present a general challenge for those already struggling.
In our current climate with COVID-19, I’ve seen through my work that social isolation has taken a significant toll. From the single parents struggling with a new mental health diagnosis and trying to return to work while also home-schooling a young child, to those in the high-risk category who found it harder to access group treatments or community programs, or worse, had to isolate completely from family members who were frontline workers.
Perception and availability of support is fluid and always changing – with significant changes often occurring following an injury. We should challenge the conception “that this is just the way it is”.
3. Financial Pressures, Housing and Food
Following an injury, it is common for finances to be impacted. In the case where the injury occurred as a result of work, the injury management system ensures the person receives financial benefits from insurers under the workers compensation scheme, or if the injury happens outside of work, they may be required to take paid, or unpaid personal leave, or they may lose their job all together.
It’s always important to consider the nature of financial distress as this influenced a number of our basic human needs. Maslow’s Hierarchy of Needs is a great example of the impact of finances:
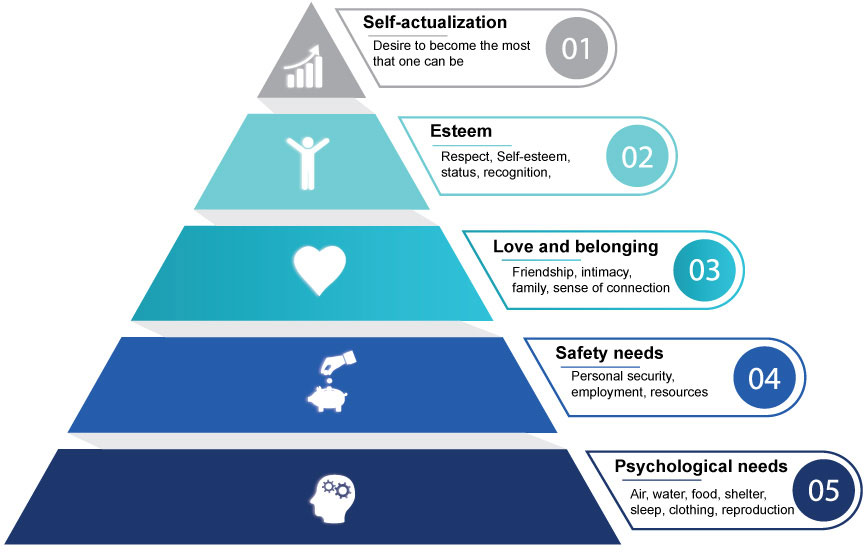
Before we even consider employment, our physiological needs must be met – this includes access to food and shelter, both things we cannot access in today’s society without financial means. If our finances are impacted by an injury, we may find ourselves struggling to make ends meet and this is likely to become the immediate priority.
One would assume in this case that the best way to address this would be via a return to work, right? To an extent, you’re right, but what happens if you can’t return to work? What happens when you spend all day and all night struggling to figure out where to go next, what happens when you can’t pay rent, what happens if your family (your kids!) end up on the street?
From a holistic, psychosocial approach to injury management it’s important to understand these areas and the influence they may have on a return to work, and general recovery.
4. Stress, Resilience and Coping
Everyone experiences stress in their lives, but we are only built to deal with so much of it. The graph below represents the stress performance curve and shows the impact of different levels of stress.
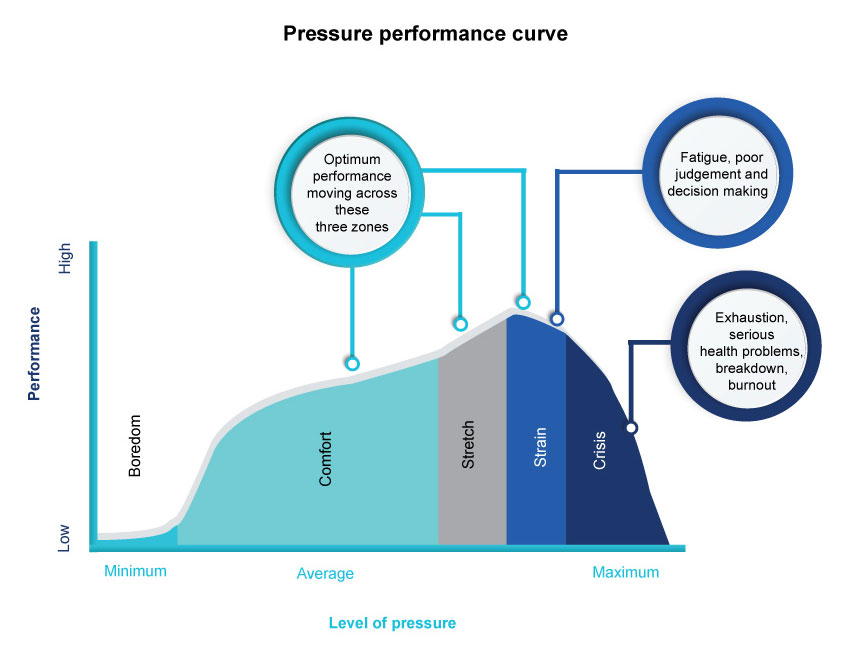
In injury management and through the process of workplace rehabilitation stress levels can impact on timeframes for return to work or, performance in the workplace following this return. The graph shows zones in which we experience an optimum level of stress (this applies to both work and homelife). When a person is injured this adds an additional layer of stress which can tip the balance in their coping. Depending on their pre-injury resilience and coping mechanisms, this may move them from the comfort zone to the stretch zone, or from strain to crisis.
What is Resilience?
Resilience is the ability for a person to bounce back following adversity (in this case, injury). Resilience is not an inherent trait, but rather a learned skill which requires ongoing strengthening and reinforcement. We run the risk of assuming someone is “a resilient person” if we do not consider their individual context and history, people who have never experienced adversity may never had been given a chance to develop skills to cope. Those that have been through trauma may have developed unhelpful coping skills such as avoidance which prolong absence from work, and often times delay overall recovery.

Resilience can be fostered through treatment but should not be overlooked in workplace rehabilitation. Within the injury management system people can be assisted to foster resilience by building interpersonal relationships and being provided with opportunities in which to trial newly developed skills. In my experience it has been helpful to assist injured people to identify skills they have used in the past to deal with stress and adversity (no matter how big or small). It is rare that a person has no coping skills whatsoever though a person may not be directly aware of them.
Bringing it Together
Appropriate treatment for injury is fundamental for recovery, however it’s important that we don’t forget the role of psychosocial factors when considering a return to work and recovery in injury management. As a professional working in workplace rehabilitation and injury management, I’m privileged to share other people’s journeys to recovery. Using a holistic, person-centred approach and considering the psychosocial influences provides the best opportunity for the injured person to feel heard and understood rather than letting them feel like a number, or worse, a diagnosis. It can be as simple as asking “how are you today? What’s not working for you, what is?” and being open to listen…
Every year, Lifeline runs a campaign known as “Stress Down Day”. Stress Down Day aims to raise awareness of the prevalence of stress and promote engagement in help seeking behaviours – and happiness in general! My hope is that this candid discussion of psychosocial (life) factors and their influence on recovery and injury management may inspire others to reflect on their work and life and move towards reducing stresses and increasing happiness both personally and professionally.
It’s often easy to overlook the bigger picture and ignore the unseen influences, but in doing so, we deny ourselves the chance to understand ourselves and others as the complex beings we are.
If you’d like to find out more or talk to someone else, here are some organisations that can help:
- SANE Australia (people living with a mental illness) – call 1800 187 263
- Beyond Blue (anyone feeling depressed or anxious) – call 1300 22 4636 or chat online
- Black Dog Institute (people affected by mood disorders) – online help
- Lifeline (anyone having a personal crisis) — call 13 11 14 or chat online
- Suicide Call Back Service (anyone thinking about suicide) – call 1300 659 467
Resources:
- https://www.sbmmagonline.co.uk/component/k2/item/151889-understanding-and-managing-workplace-stress
- https://mhaustralia.org/our-work/look-after-your-mental-health-australia
- https://www.sane.org/
- https://www.beyondblue.org.au/
- https://www.blackdoginstitute.org.au/
- https://www.healthdirect.gov.au/mental-illness
- https://www.suicidecallbackservice.org.au/

